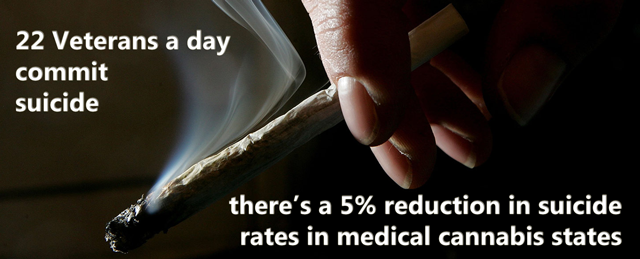
The use of cannabis (marijuana) to treat the symptoms associated with battle-field brain trauma or abuse trauma are well understood by those who suffer from psychic wounds. Symptoms of PTSD (Post Traumatic Stress Disorder) include heightened reactivity, insomnia, lack of emotional control, hyper arousal and agitation and suicidal ideation among others. Cannabis use is associated with less issues with each of these conditions. Cannabis is known as a herb with significant anti anxiety properties by the many researchers who continue to unlock the complicated neuro-chemical pathways of the endocannabinoid system (ECS).
Cannabis should be a first line treatment for PTSD symptoms unless a contraindication to cannabinoids exists. Veterans and other PTSD sufferers should understand that different strains of cannabis can produce markedly different effects. THC, the cannabinoid molecule present in greatest amount, stimulates most of the psycho-active “high” of cannabis, and patients who suffer from reactivity and agitation should be aware that THC may be contraindicated for them. High CBD strains may be more therapeutic, than high THC strains.
The activity of the main psychoactive compound in cannabis THC is biphasic in many assays. In other words, low and high doses may cause opposite effects. Three main cannabinoids THC, CBD and CBC have all been shown to exhibit significant anti-depressant effects.
Anti-depressant action of cannabis as well as the interaction between anti-depressants and the
endocannabinoid system has been reported. THC as an anti-depressant like
activity of Δ9-THC and other cannabinoids has been examined. The anti-depressant-like action of Δ9-THC, cannabidiol (CBD) and cannabichromene (CBC) has been confirmed multiple times with exhibited significant effect. Studies have shown that Δ9-THC and other
cannabinoids exert anti-depressant like actions, and thus may contribute to cannabis' overall mood-elevating
properties.
CBD as an anti-psychoticAvailable treatments for schizophrenia are only modestly effective and cause serious metabolic and neurological side effects. Therefore, there is an urgent need for novel therapeutic targets for the treatment of schizophrenia. A highly promising new pharmacological target in the context of schizophrenia is the endocannabinoid system (eCB). Modulation of this system by the main psychoactive component in cannabis, Δ9-tetrahydrocannabinol (THC), induces acute psychotic effects and cognitive impairment.
However, the non-psychotropic, plant-derived cannabinoid agent cannabidiol (CBD) may have antipsychotic properties, and thus may be a promising new agent in the treatment of schizophrenia. Cannabidiol modifies the effects of THC. Thus, CBD blocks anxiety provoked by THC. Studies have investigated and confirmed the antipsychotic properties of CBD in human subjects. Results show the ability of CBD to counteract psychotic symptoms and cognitive impairment associated with cannabis use as well as with acute THC administration. In addition, CBD may lower the risk for developing psychosis that is related to cannabis use.
The first small-scale clinical studies with CBD treatment of patients with psychotic symptoms further confirm the potential of CBD as an effective, safe and well-tolerated antipsychotic compound.
- Depression
- PTSD
- ADHD
- Schizophrenia
The activity of the main psychoactive compound in cannabis THC is biphasic in many assays. In other words, low and high doses may cause opposite effects.
Treating depression with cannabis therefore takes careful consideration, as too much of the herb may result in the opposite to the intended effect.
Repeated studies have shown that cannabis use persists among post-traumatic stress disorder sufferers as a means of coping with their psychological symptoms.
The classic symptoms of PTSD include frequent panic attacks in response to triggers that keep a person always on the edge and physically and mentally stressed out, disturbed sleep, and recurring nightmares. Since cannabis use faciliates sleep it is not hard to understand why PTSD suffered cling to cannabis.
The data for treating ADHD with cannabis is muddled. Studies have suggested that people with ADHD who used cannabis daily were more likely to have the hyperactive and impulsive symptoms of ADHD, rather than the inattentive symptoms.
So marijuana helped manage the hyperactivity and impulse control struggles that come with that form of ADHD. But other studies have different results.
Cannabis can precipitate anxiety attacks or even schizophrenia in susceptible individuals. Patients at risk of schizophrenia and psychotic breaks should not use cannabis.
Despite this it is interesting to note that surprisingly, the extent of schizophrenia in the general population does not seem to have increased in parallel with the very wide use of cannabis for recreational purposes.

 Depression & Cannabis
Depression & Cannabis